When it comes to treating periodontitis, it’s crucial to understand the best medication options available. Periodontitis is a serious gum infection that damages the soft tissue and destroys the bone supporting your teeth. Without proper treatment, it can lead to tooth loss and other health complications.
Recent studies have shown that a combination of antibiotic therapy and regular dental cleanings can be highly effective in managing periodontitis. By understanding the best medication for periodontitis, you can take proactive steps towards improving your oral health and overall well-being.
Understanding the Benefits of Antibiotic Therapy
Antibiotic therapy is a crucial treatment option for bacterial infections. Understanding the benefits of antibiotic therapy can help individuals make informed decisions about their healthcare. One popular and reliable resource for information on antibiotics is the website of the Centers for Disease Control and Prevention (CDC). Here, you can find detailed guides on different types of antibiotics, their uses, and potential side effects.
To access the CDC website and learn more about antibiotic therapy, follow these steps:
- Open your web browser and type in www.cdc.gov
- Once on the CDC homepage, navigate to the “Antibiotic Resistance” section
- Click on the “Antibiotic Prescribing and Use” tab for comprehensive information
Exploring the Effectiveness of Regular Dental Cleanings
Regular dental cleanings are essential for maintaining oral health and preventing gum disease. Exploring the effectiveness of regular dental cleanings can shed light on the importance of consistent dental hygiene practices. One useful platform to gather insights on dental cleanings is the American Dental Association (ADA) website. Here, you can find articles, videos, and expert advice on the benefits of regular cleanings.
To access the ADA website and delve into the effectiveness of regular dental cleanings, follow these simple steps:
- Visit www.ada.org using your preferred web browser
- Navigate to the “Oral Health Topics” section on the homepage
- Select the “Prevention” category and click on “Regular Dental Visits” for detailed information
Choosing the Right Medication for Periodontitis
Selecting the appropriate medication for periodontitis is crucial for effectively managing this dental condition. Understanding how to choose the right medication can improve treatment outcomes and overall oral health. One reputable source for medication information is the National Institute of Dental and Craniofacial Research (NIDCR) website. Here, you can find research-based recommendations on periodontitis medications.
To access the NIDCR website and learn more about choosing the right medication for periodontitis, follow these steps:
- Go to www.nidcr.nih.gov using any web browser
- Explore the “Research” section and look for “Periodontal Disease Studies”
- Click on the relevant study to access detailed information on medication options
Exploring Innovative Approaches to Periodontitis Therapy
When it comes to treating periodontitis, exploring innovative approaches is crucial for effective management. One such approach involves the use of targeted antibiotic therapy to address specific pathogens associated with gum disease. By identifying the bacteria responsible for the infection, clinicians can tailor antibiotic treatment to achieve optimal results. This personalized approach not only enhances the efficacy of the treatment but also helps minimize the development of antibiotic resistance.
Another innovative strategy for periodontitis therapy is the use of host modulation therapy. This approach focuses on modifying the host response to bacterial infection, rather than targeting the bacteria directly. By regulating the inflammatory pathways involved in gum disease, host modulation therapy can help reduce tissue destruction and promote better healing outcomes. Incorporating this approach into the overall treatment plan can lead to more comprehensive and sustainable results.
Furthermore, advancements in regenerative medicine have opened up new possibilities for treating periodontitis. Techniques such as tissue engineering and growth factor delivery can support the regeneration of damaged periodontal tissues, promoting long-term structural and functional restoration. By harnessing the body’s natural healing mechanisms, these regenerative approaches offer promising solutions for addressing the underlying causes of gum disease.
In addition to traditional periodontal therapies, innovations in laser technology have revolutionized the treatment of periodontitis. Laser-assisted periodontal therapy allows for precise and minimally invasive interventions that target bacteria and diseased tissue while preserving healthy surrounding structures. This approach offers faster healing times, reduced discomfort, and improved treatment outcomes for patients with periodontal issues.
Overall, exploring innovative approaches to periodontitis therapy is essential for advancing the field of periodontology and improving patient care. By embracing cutting-edge techniques and technologies, clinicians can tailor treatment plans to the specific needs of each individual, resulting in more effective and sustainable outcomes in the management of gum disease.
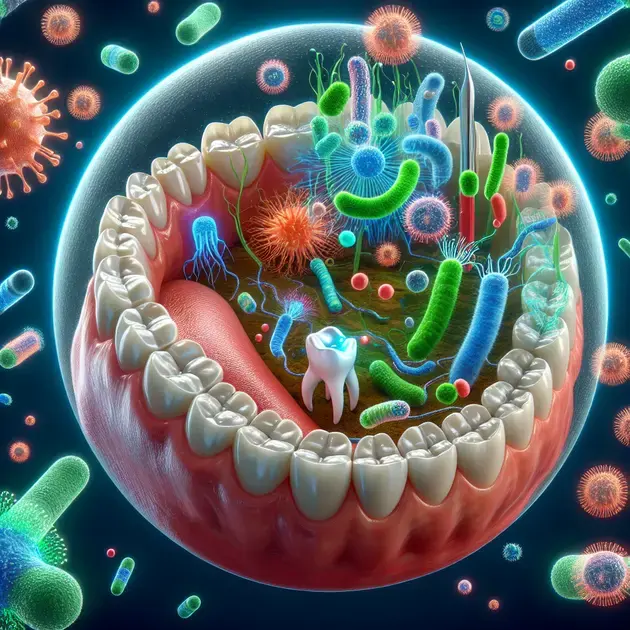
Understanding the Connection Between Oral Microbiome and Gum Health
The oral microbiome plays a pivotal role in maintaining gum health and preventing periodontal diseases. This complex ecosystem of bacteria, fungi, and viruses interacts with the host’s immune system to maintain a delicate balance that is essential for oral health. Disruption of this balance can lead to dysbiosis, an imbalance in the oral microbiome, which is associated with the development of gum diseases such as periodontitis.
Recent research has highlighted the intricate relationship between specific microbial species and periodontal health. Pathogens such as Porphyromonas gingivalis and Treponema denticola have been identified as key players in the progression of periodontitis. Understanding how these bacteria interact with the host tissues and immune system is crucial for developing targeted therapies that address the underlying causes of gum disease.
Furthermore, studies have shown that certain probiotic strains can help restore microbial balance in the oral cavity and support gum health. Probiotics such as Lactobacillus reuteri and Bifidobacterium animalis have demonstrated potential in reducing inflammation, inhibiting pathogen growth, and promoting tissue regeneration in the periodontal environment. Incorporating probiotics into oral care routines may offer a natural and safe way to support oral microbiome balance and prevent gum diseases.
Optimizing Personalized Treatment Plans for Gum Disease Management
Personalized treatment plans are essential for optimizing the management of gum disease and enhancing treatment outcomes. By tailoring interventions to the specific needs and characteristics of each patient, clinicians can address the unique factors contributing to the development and progression of periodontal diseases. This individualized approach ensures that patients receive the most effective and appropriate care for their oral health concerns.
One key aspect of personalized treatment plans for gum disease management is risk assessment. By evaluating factors such as oral hygiene practices, medical history, genetic predisposition, and lifestyle habits, clinicians can identify individuals at higher risk for developing periodontitis. This proactive approach allows for early intervention and preventive measures to mitigate the progression of gum disease.
Furthermore, integrating advanced diagnostic tools such as oral microbiome analysis and genetic testing into treatment planning can provide valuable insights into the underlying causes of gum disease. Understanding the microbial composition of the oral cavity and genetic susceptibility factors can help tailor treatment strategies that target the root causes of periodontitis, leading to more successful outcomes.
In addition, patient education and engagement play a critical role in optimizing personalized treatment plans for gum disease management. By empowering patients to take an active role in their oral health through proper oral hygiene practices, lifestyle modifications, and regular follow-up visits, clinicians can enhance treatment compliance and long-term treatment success. Building a collaborative relationship with patients based on mutual trust and open communication fosters better treatment outcomes and overall oral health improvement.
Conclusion
Exploring innovative approaches to periodontitis therapy is crucial for advancing patient care in the field of periodontology. By incorporating targeted antibiotic therapy, clinicians can tailor treatments to address specific pathogens associated with gum disease, enhancing efficacy while minimizing antibiotic resistance development. Host modulation therapy offers a unique strategy by focusing on regulating inflammatory pathways to reduce tissue destruction and promote healing outcomes, leading to more comprehensive results in treatment plans.
Advancements in regenerative medicine, such as tissue engineering and growth factor delivery, present promising solutions for supporting the regeneration of damaged periodontal tissues. These techniques harness the body’s natural healing mechanisms to address the underlying causes of gum disease, promoting long-term structural and functional restoration. Laser technology innovations in periodontitis treatment provide precise interventions that target bacteria and diseased tissue, offering faster healing times and improved outcomes for patients.
Understanding the connection between the oral microbiome and gum health is essential for preventing periodontal diseases. By recognizing the intricate relationship between specific microbial species and periodontal health, targeted therapies can be developed to address the root causes of gum disease. Incorporating probiotics like Lactobacillus reuteri and Bifidobacterium animalis into oral care routines can help restore microbial balance, reduce inflammation, inhibit pathogen growth, and promote tissue regeneration, supporting overall oral microbiome balance.
Optimizing personalized treatment plans for gum disease management is key to enhancing treatment outcomes and patient care. By tailoring interventions through risk assessment and advanced diagnostic tools, clinicians can address the unique factors contributing to periodontal diseases. Empowering patients through education and engagement in their oral health practices fosters better treatment compliance, long-term success, and overall improvement in oral health outcomes.



